How to create behaviour change in patients with diabetes through healthcare UX design
A look at how UX design can be used in digital therapeutics app development to improve treatment adherence in patients with diabetes or other chronic illness management.
This post is a summary of a talk by speaker Sille Clara Nielsen’s given at the UX healthcare Berlin 2022 conference, she presented her key findings for behaviour modification in diabetes patients through UX design.
I had the chance to attend the UX Healthcare Berlin conference (organised by UX Healthcare) in September 2022, I was pleasantly delighted to learn how folks are using UX design to improve health outcomes. The speaker Sille Clara showcased a great example of how a digital therapeutics app have the potential to enhance the lives of diabetes patients through simple UX design elements, such as adding symbols or reducing the number of notifications. Good UX design in digital therapeutics could open doors for new possibilities in chronic illness management, and the prospect excites me.
Below, I share key takeaways from the event ‘Designing for real, not ideal behaviour. The importance of UX in therapeutics’ by Sille Clara Nielsen.
What are digital therapeutics?
A digital therapeutics apps are evidence-based therapeutic interventions backed by sophisticated software programs that can help prevent, manage, and treat chronic illnesses.
Prescription digital therapeutics (PDT) apps are in very early stages of use in clinical practice but offer the potential to improve the lives of patients living with chronic illnesses. While promising, these apps come with a huge burden of responsibility; there’s limited scope for error as digital therapeutics interact with vulnerable people’s lives. As UX designers we have to be empathic and take a care-based approach to designing a therapeutic application.
How digital therapeutics can be important in managing chronic illnesses
Sille's talk had some eye-opening statistics that got my attention and gave me some pause. For example, apparently 4% of pregnant women develop gestational diabetes, while 50% of the women are at risk of developing Type 1 diabetes within ten years after pregnancy. It is alarming to learn the prevalence of an illness with no real cure, if you apply the Rule of Halves it means the situation maybe way worse than expected. Out of 387 million people with diabetes, only 50% are diagnosed, 50% receive proper care, and only 50% can achieve the desired outcome. PDTs have the potential to increase the amount of people who receive care and achieve desired outcomes.
See the screenshot below.
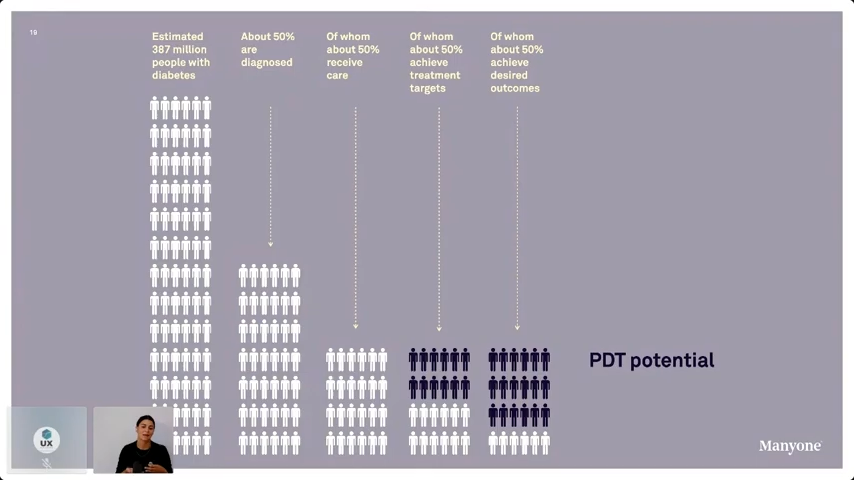
Research from the International Diabetes Federation says 643 million adults may develop diabetes by 2030 and 783 million by 2045. This information only points to a future where more patients will need assistance, and due to the labour shortages we are seeing in healthcare it won't be possible to provide care without digital therapeutics.
The problem: challenges of chronic illness management
A reason why so many people do not receive the necessary diagnosis or aren’t able to get treatment is that they are not able to adhere to treatment plans. Healthcare UX designers in digital therapeutics can help solve for adherence through easy-to-use experiences and interfaces with clear easy to follow actionable treatment plans.
For example, the speaker worked on a project with a global pharmaceutical company to design a digital therapeutic app that assisted patients with diabetes in the initiation phase of insulin treatment. The app was designed to help patients adjust their doses based on their individual needs. However, the patients still required the doctor's guidance. Nielsen and her team are working to enhance the app to enable self-administration, helping patients become independent in their diabetes treatment and to help patients become independent in their treatment, which is crucial to design for behaviour modification.
about-sheda
How to Design for behaviour change
Healthcare UX designers should focus on 'real' behaviour rather than 'ideal' behaviour. Ideal behaviour is based on the assumption that patients will behave according to the plan, which is not the case.
“We are designing for behaviour change,” Sille said. “No human can be 100% adherent. And it’s not because people are incapable of adhering; they don’t know what to do. And in some cases, life happens; something gets in the way.”
This reminded me of this funny meme that illustrates the difference between ideal and real behaviour.

She outlined 5 ways UX design that can assist in helping patients alter their behaviour and stay on course for treatment. These are listed below.
1. Minimise the number of interactions and time spent on the application
Diabetes is a scary illness; it has no cure, so patients have a lot to deal with and learn once they are diagnosed . To help patients stay on track, healthcare UX designers must remove any needless information from the interface that the customers have not asked for. Keep the interfaces ambiguity-free with necessary notifications only. The goal should be to have gentle reminders, not a constant bombardment of messages, so the patient does not feel overwhelmed.
2. Use simple words
Identify words patients are already using and use them in application interfaces. For example, people use the word sugar, not glucose.
Similarly, it’s hard for people to understand subcutaneous allergen immunotherapy, I'm not sure I would be to say it if asked.
Consider using intuitive symbols or icons within the interface, these prompt patients to look into unknown or difficult words related to the illness.
3. Do bite-sized onboarding
UX designers should remember that the goal is to empower patients so they can treat themselves by trusting and relying on the application. But that is only possible if patients are willing to sign up. To make this easier, provide information in bite-sized burst to not overwhelm them.
“Do not give too much information to the patients in the early stage,” Sille suggests . “Understand that the patients are learning to cope with the disease while trying to manage it. Don’t overwhelm them.”
Give information like 'dose size' or 'how to inject' in intervals.
4. Identify key learning moments
Another aspect of helping consumers trust your application and adhere to the treatment plan is recognising moments when patients need help.
Healthcare UX designers need to identify specific moments when patients will have questions and offer an immediate remedy for that situation. For example, if a user is experiencing fear-driven reluctance for a higher dose, tell them through a notification or a pop-up that healthcare practitioners approve of higher dosing. It could be: "This dosage has been clinically approved."
5. Design for when things go wrong
A high percentage of patients will not be fully adherent to the course of treatment outlined for them. Therefore, UX designers need to design for when patients are not on track. The best way to achieve this is by minimising guilt or shame and guiding patients to what small steps they can carryout to get back on track. In other words, rather than focusing on what they didn’t do, focus on what they can do in their unique scenario.
Conclusion
All in all, it was a very informative session. I learned about the intricate details within UX design that could make or break the application. I heard someone voice their concern about the questionnaire the patients have to fill out during the onboarding process and how it may discourage them from signing up.
Below, I am summarising some takeaways on what to think about when designing for behaviour change in a healthcare app.
1. Notifications are necessary, but you can't rely on them alone. Use them sparingly. UX designers should use other channels, including emails, to communicate.
2. Educate patients about managing their chronic illnesses through bite-sized information. Try not to overwhelm the patient with too much information at once.
3. Use encouraging words like “Success" or "well done!” during the onboarding process to ensure patients do not get bored or tired of the long questions. In addition, only ask the most important questions.
At the end of her talk, Nielsen seemed optimistic about the future of PDT despite the regulations that may hinder its progress. If we can design therapeutic applications that help patients modify behaviour and stay on course, we can not only change people’s lives but empower them to participate in their communities as healthy individuals capable of achieving enumerable success.
If you are an optimistic healthcare practitioner or provider interested in utilising human-centered design and innovative technological solutions to create digital therapeutics apps to better manage chronic illnesses and improve the healthcare outcomes of your patients, reach out to me for a chat.
At Sheda, we can guide you through the process of designing and developing apps that improve healthcare outcomes. Drop me a line below or click on the floating head to chat with me.